Economics of Infant Feeding in the U.S.
Duke University
The Issue:
The national shortage of baby formula in the U.S. that began in February of 2022 cast an urgent spotlight on the difficulties parents can face in meeting basic nutritional needs of their babies. Strains on formula supply chains induced by the COVID pandemic were greatly exacerbated by a voluntary formula recall by Abbott Nutrition and the months-long closure of a major formula production facility in Sturgis, Michigan. The crisis not only raised questions about the regulation and market structure of the formula industry but also prompted calls for broader reliance on breastmilk and to increase supports available to breastfeeding parents, especially given the gap between recommendations and practice. For example, less than a quarter of U.S. infants meet the American Academy of Pediatrics’ recommendation of exclusive breastfeeding for the first 6 months of life. However, the narrow focus on the supply of infant formula, or on specific AAP recommendations, does not shed light on the full scope of economic tradeoffs families face when deciding how to best ensure the nutritional health of their infant.
A narrow focus on the supply of infant formula or the benefits of breastfeeding does not shed light on the full scope of economic tradeoffs families face.
The Facts:
- Deficiencies in early nutrition can have long-term consequences. It is recommended that infants should only consume either breastmilk or formula during the first six months of life, with health authorities including the World Health Organization and the U.S. Centers for Disease Control and Prevention strongly favoring exclusive breastfeeding during this time. Breast milk has unique nutritional properties, such as the ability to transfer maternal antibodies, and studies suggest multiple infant and maternal health benefits; however, the direct causal link between breastfeeding and children’s early health in a developed country context such as the U.S. is challenging to identify. Nevertheless, some recent evidence from the United Kingdom shows that breastfeeding improves cognitive development among infants of mothers with lower levels of education. Food security during children’s earliest years of development matters to subsequent infant health risks, with early nutritional deficiencies and malnutrition potentially having irreversible, lifelong consequences for children's subsequent neurodevelopment and cognitive functioning. Human milk naturally provides many important macro- and micronutrients; infant formula is designed to mimic human milk to provide these nutrients
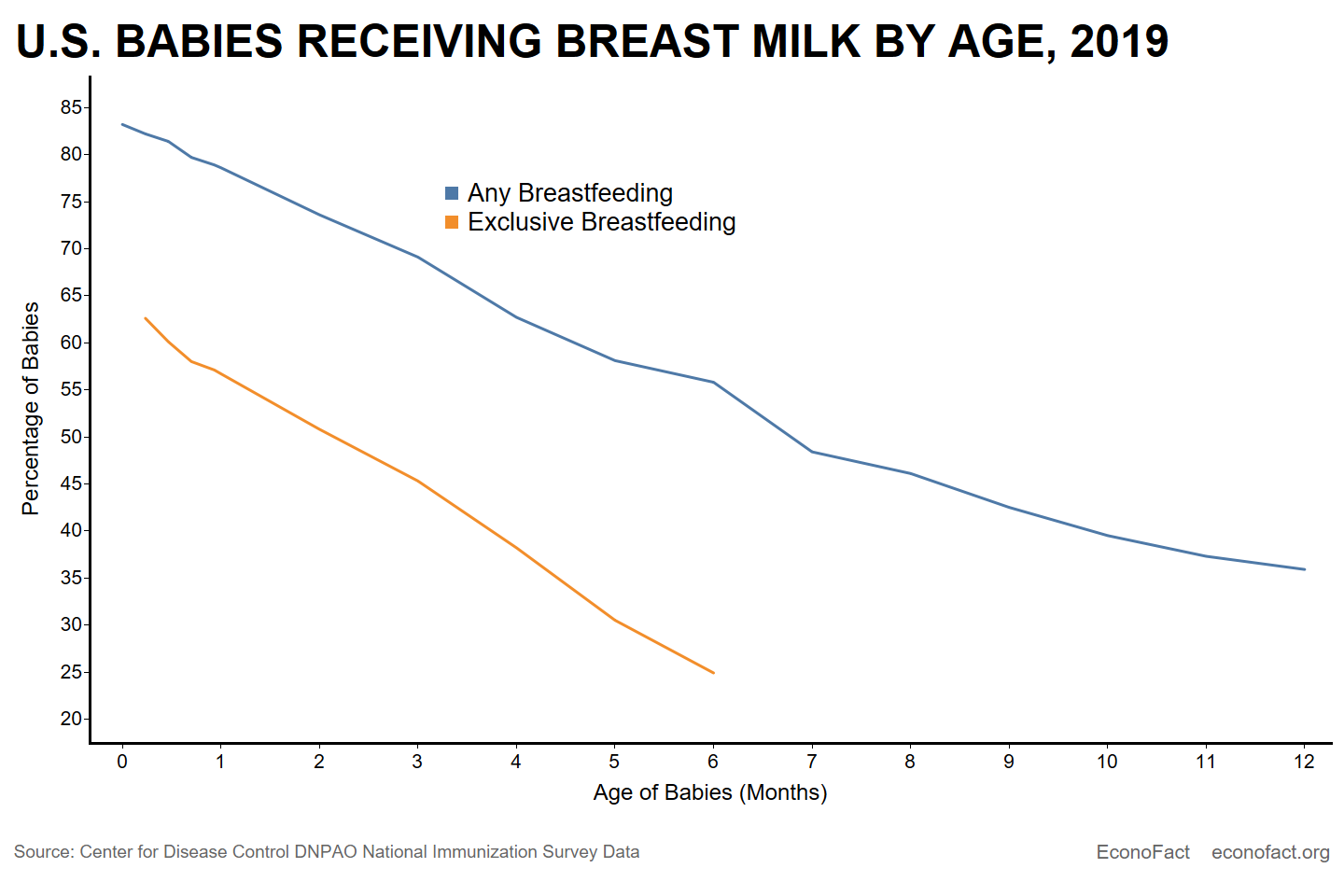
- Many mothers in the United States start to breastfeed but the share of infants receiving breastmilk decreases markedly over time and varies widely across family socioeconomic characteristics. A majority of mothers, about 84%, report ever breastfeeding in the most recent survey data available. However, few are able to adhere to the AAP guidelines, with only about a quarter of mothers reporting exclusive breastfeeding through 6 months (see chart). Higher levels of poverty are associated with lower rates of breastfeeding: About 40% of mothers living below the poverty level report any breastfeeding at 6 months. In contrast, about 70% of mothers whose income is greater than six times the poverty level report some breastfeeding at 6 months, according to CDC data. Mothers who are younger, have lower levels of education, or are unmarried also report lower shares of infants receiving any breastmilk at 6 months (see here).
- Financial and social support for breastfeeding is mixed, and uneven, in the U.S. While breastfeeding predominated in the 19th century, infant feeding practices changed dramatically between the 1880s and the 1940s in the United States towards a broad acceptance of medically-directed artificial infant feeding (see here). Breastfeeding rates reached their lowest point in the 1970s and rates have been rising since then; however, this means that many women do not have mothers or relatives who they can turn to for breastfeeding advice as people did back in the 18th and 19th centuries for example. Breastfeeding support, counseling and equipment are covered under many health insurance plans but even for women with a primary care physician or pediatrician, the supply of skilled lactation consultants is low. There are an estimated 5.1 Internationally Board Certified Lactation Consults (IBCLCs) per 1,000 live births in the U.S., falling below the recommended standard of 8.6 per 1,000 live births, and many pediatricians report feeling ill-prepared to provide breastfeeding support to lactating parents. Access to professional lactation support can be critical; many mothers stop breastfeeding earlier than intended due to lactation difficulties and concerns about milk supply. Hospitals play an important role in establishing infant feeding practices. However, the U.S. does not adhere to international standards on formula marketing, enabling formula companies to use aggressive marketing strategies, such as encouraging healthcare workers to distribute free samples to parents. Slightly over a quarter of all U.S. births occur in hospitals designated “Baby-Friendly,” which is viewed as the gold standard for infant feeding practices. Inequities persist in hospital offerings; Black infants are more likely to be introduced to formula during their hospital stay and maternity facilities that follow baby-friendly practices are less prevalent in neighborhoods with a higher percentage of Black residents.
- Formula may be costly, but breastfeeding is not “free.” Advocates for breastfeeding cite the high cost of formula, with savings of up to $1,500 in direct infant formula costs. This line of argument does not consider the opportunity costs of breastfeeding, including the potential direct loss of wages from taking breaks to express breast milk at work, the time investment required to breastfeed and/or pump milk, and breastfeeding supplies, including special storage bags or clean, food-grade containers to store pumped milk, nursing bras, etc. For the first few weeks, infants breastfeed 8-12 times per day. Assuming an infant breastfeeds for 20-40 minutes per feed, the time cost of breastfeeding for a lactating parent making federal minimum wage would be between $588-$1,765 in the first month alone.
- Many mothers in the U.S. are faced with difficult decisions between breastfeeding and paid work. Mothers who return to work full-time and/or shortly after giving birth are less likely to plan to exclusively breastfeed, have lower rates of breastfeeding initiation, and have shorter breastfeeding durations. On the other hand, increased paid family leave has been shown to increase breastfeeding duration and the likelihood of breastfeeding for at least 6 months (see here), yet only about 50% of U.S. mothers who are working at the time of birth report taking some paid leave. Lactating parents who return to work and breastfeed are often met by a lack of professional support. Provisions from the 2010 Patient Protection and Affordable Care Act amended Section 7 of Fair Labor Standards Act (FLSA) such that employers are required to provide “reasonable break time” and “a place, other than a bathroom, that is shielded from view and free from intrusion from coworkers and the public” for employees to express breast milk excludes an estimated 9 million workers of childbearing age who are exempt from Section 7 of the FLSA, which includes the majority of salaried employees (see here). A recent bill – the PUMP Act – would have expanded protections to salaried employees but failed to pass the Senate in June 2022 during the height of the formula shortage; a similar bill – the Pregnant Workers Fairness Act – remains sitting in the Senate.
- Formula can play an important role in supporting infant nutrition, but availability and cost is vulnerable to shocks. A recent Econofact podcast examined the supply side factors that contributed to the infant formula shortage, including market consolidation (four producers – Abbott, Mead-Johnson, Perrigo, and Nestlé - control approximately 90% of the formula market), high tariffs on imported formula leading to a reliance on domestic producers, and ongoing supply chain issues due to COVID-19. These factors contributed to increasing formula prices and out of stock percentages prior the shutdown of Abbott’s Sturgis, Michigan plant in February 2022, which substantially exacerbated these issues. The shutdown of the Sturgis plant demonstrated the fragility of the formula market to supply shocks: formula prices increased by an average of 11% between March 2021 and May 2022 and shortages spiked to over 74% nationwide at the end of May 2022, with ten states having shortage levels of 90% or greater. At the same time, the industry’s profit margin increased by 2.6 percentage points. To address the shortage, Congress passed legislation to temporarily suspend tariffs on infant formula (see here) and more recently, legislation to suspend tariffs on formula based power used in the manufacturing of formula in the U.S. (see here). Both expire on December 31, 2022. The long-term welfare implications of the Cronobacter contamination and the infant formula shortage remain unknown. The Cronobacter sakazakii bacteria that led to the Sturgis plant shutdown is one of the few organisms that can survive in powdered formula and can cause severe meningitis. Because there is currently no comprehensive mechanism for detecting or investigating Cronobacter infections, infant formula production remains vulnerable to future outbreaks and shutdowns. The shortage also had negative implications for infant’s health as some families turned to rationing supplies or creating homemade formula to deal with the crisis.
- The federally funded Women, Infant and Children (WIC) program can play a role in the supply and availability of formula in different states and in influencing infant feeding decisions for low-income families. WIC is one of the most successful early intervention nutritional supports with high take up and demonstrated benefits to infants and young children. Breastfeeding promotion is a central goal of the WIC program, with state and local agencies required to create procedures to ensure breastfeeding support for beneficiaries, staff trained on breastfeeding promotion, and more generous food packages offered to fully or partially breastfeeding moms. The White House recently announced testing of telehealth initiatives to provide virtual breastfeeding support and one-on-one counseling through the WIC program. However, breastfeeding rates among WIC participants remain below the national average, with participants citing lack of support at home, need to return to work, and lack of time as barriers to breastfeeding. As such, approximately half of all infant formula sold in the U.S. is purchased with WIC benefits. WIC has sole source contracts with formula manufacturers receiving rebates that reduce costs, which allows WIC to serve more eligible families but also limits the types of formula beneficiaries can obtain. In response to the supply crisis, Congress passed legislation (see here) that waives restrictions on the type of formula WIC recipients can purchase and on the maximum monthly allowance for formula during a product recall or supply chain crisis.
What this Means:
Infants who do not consume the necessary micronutrients early in life may face risks to healthy development. While the nutritional value of breastmilk is high and mothers seem to have internalized the “breast is best” mantra, this recommendation is wildly in conflict with policy support available for mothers (and, families more broadly), and also not aligned with industry drivers for the production and marketing of infant formula. Many working families do not have paid parental leave, protections for lactating parents to express milk at work is limited, and availability of lactation consultants and cost coverage for breastfeeding supports (e.g., pumps) is far from universal. Even though over 90 percent of births occur in hospitals, birthing hospitals offer mixed support for breastfeeding. Infant feeding choices are particularly constrained for low-income mothers who work in jobs where they are unable to pump, which may explain some of the stark inequities in breastfeeding rates by race and socioeconomic status. A majority of U.S. babies rely to some extent on formula to meet their nutritional needs and, as the recent crisis highlighted, further action is necessary to ensure the safety of the product and the resiliency of the market to future supply shocks.
Like what you’re reading? Subscribe to EconoFact Premium for exclusive additional content, and invitations to Q&A’s with leading economists.